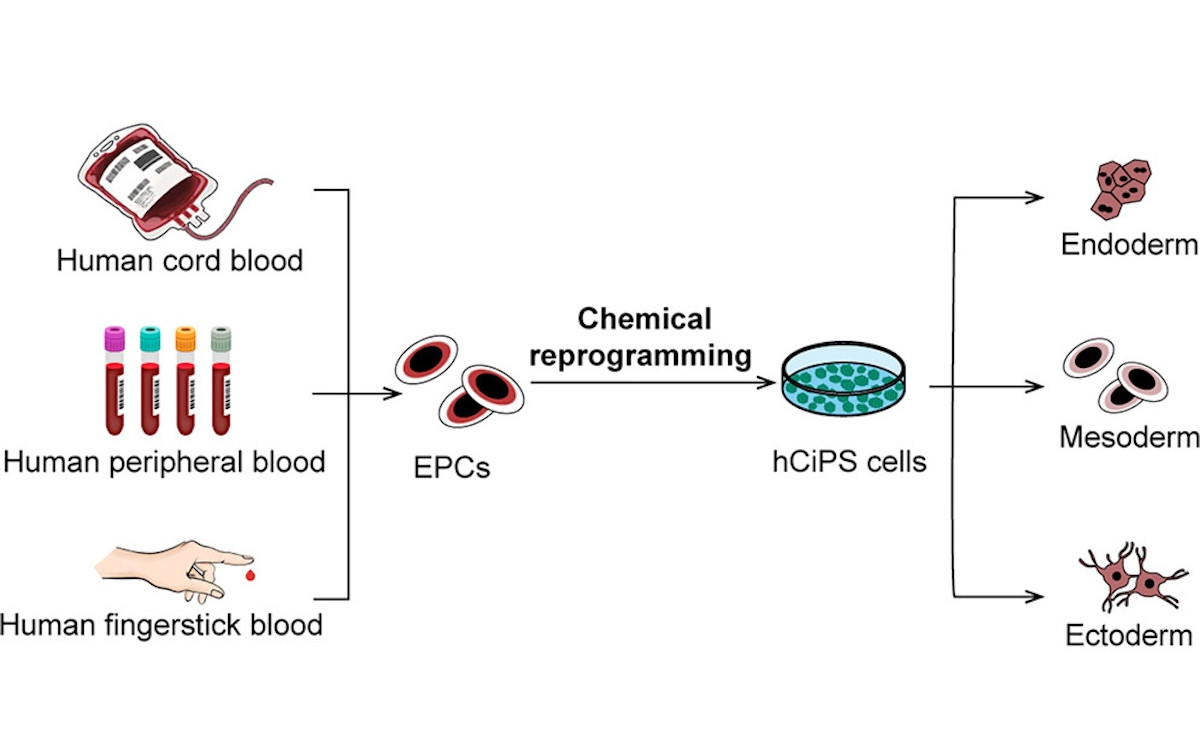
Imagine creating stem cells capable of becoming any cell type in the human body—from nothing more than a single drop of blood. This is no longer science fiction. In a landmark study published in Cell Stem Cell (August 2025), a team led by Hongkui Deng at Peking University unveiled a robust, fully chemical method to reprogram human blood cells into pluripotent stem cells—without using genetic modification.
Why This Matters
Pluripotent stem cells (PSCs) are the master builders of biology. They can differentiate into heart cells, neurons, pancreatic islet cells, and more, making them invaluable for disease modeling, drug discovery, and potential therapies. Until now, generating them from human blood—a readily accessible and minimally invasive source—has been challenging, especially without introducing foreign genes.
The Deng lab’s approach changes that. Their human chemically induced pluripotent stem cells (hCiPS cells) are made using only small molecules, eliminating the need for viral vectors or transcription factor delivery. This could make stem cell generation safer, cheaper, and more scalable.

The Breakthrough
Using both cord blood mononuclear cells (CBMCs) and adult peripheral blood mononuclear cells (PBMCs), the researchers optimized a stepwise chemical “reprogramming cocktail” that:
- Erases blood cell identity by targeting signaling pathways and epigenetic regulators.
- Activates early developmental programs, including the key stem cell gene LIN28A.
- Produces colonies expressing pluripotency markers (OCT4, SOX2, NANOG).
The results are striking:
- Over 200 hCiPS colonies per well from cord blood in just 20 days.
- Works with both fresh and cryopreserved samples, even those stored for over 4 years.
- A single fingerstick (50–100 µL of blood) can yield 50–100 hCiPS colonies with a 100% success rate.
Even more impressively, the chemical method was over 20× more efficient than conventional transcription factor–based approaches for blood cells.
Quality and Potential
The hCiPS cells generated showed:
- Gene expression and epigenetic patterns highly similar to human embryonic stem cells.
- No residual “somatic memory” from their blood origins.
- The ability to form derivatives of all three germ layers in vitro and in vivo.
- Directed differentiation into therapeutically relevant cell types, including pancreatic islets, neural stem cells, hepatic progenitors, and hematopoietic cells.
The team notes that such cells could, in principle, be banked and used for personalized cell therapy, disease modeling, or drug screening—without the safety concerns of integrating genetic material.
Beyond the Lab
Chemical reprogramming isn’t new, but applying it robustly to human blood cells marks a major milestone. Compared to older methods, it’s:
- Non-genetic – no risk of insertional mutagenesis.
- Scalable – small molecules are easy to synthesize and standardize.
- Accessible – requires only a small blood sample.
The implications span from building global iPSC libraries from stored blood samples, to point-of-care regenerative kits for hospitals, to unlocking new avenues for rare disease research.
Looking Ahead
While the study shows strong reproducibility, the authors acknowledge that further work is needed to fully assess long-term genomic stability and optimize the protocol. Still, the prospect of generating clinical-grade stem cells from a painless finger prick is a transformative step toward democratizing regenerative medicine.
As Deng and colleagues’ work makes clear, the future of personalized cell therapy may be as simple as rolling up your sleeve.
Reference:
Peng F., Wang Y., Cheng L., et al. (2025) Chemical reprogramming of human blood cells to pluripotent stem cells. Cell Stem Cell, 32(8), 1–8. https://doi.org/10.1016/j.stem.2025.07.003