A New Horizon in Type 1 Diabetes—Replacing Beta Cells
Introduction
Type 1 diabetes—a condition marked by the immune‑mediated destruction of insulin‑producing beta cells—has long relied on insulin injections as the only means to survive. A groundbreaking shift may be emerging, as the latest NEJM editorial, “Replacement of Beta Cells for Type 1 Diabetes,” unveils the scientific groundwork underpinning two novel cellular strategies toward regenerating these vital cells (New England Journal of Medicine).
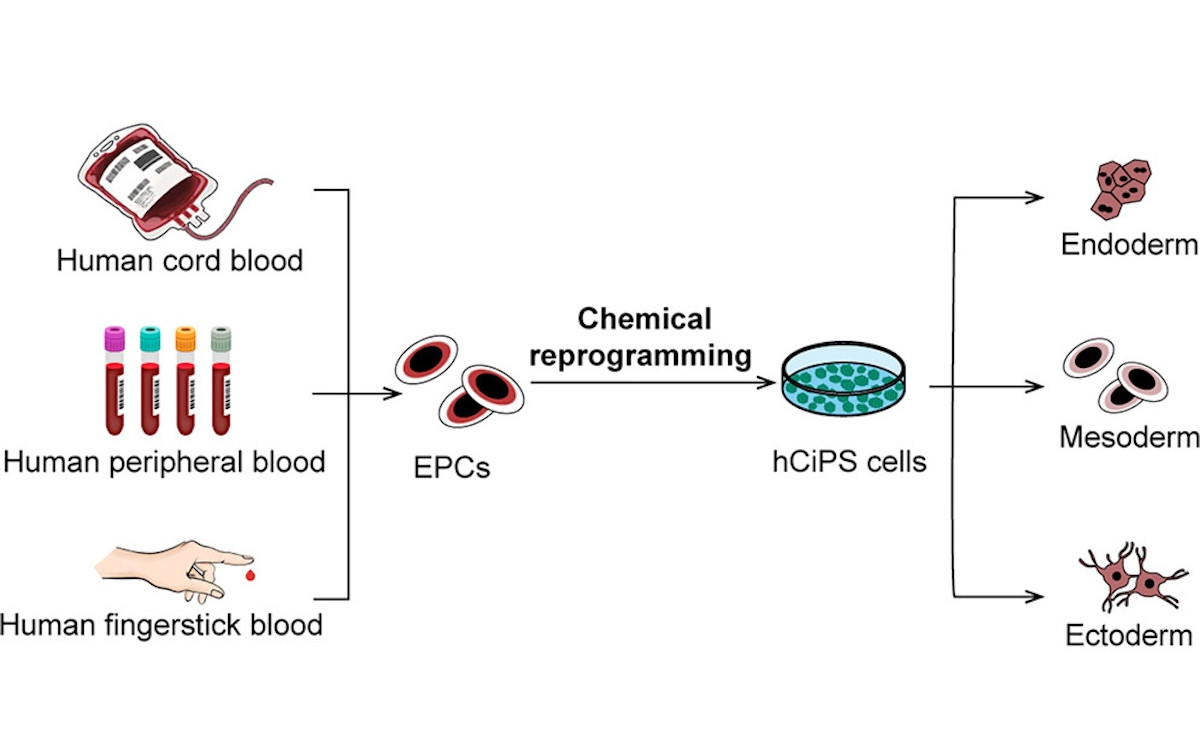
1. Stem Cell-Derived Islets (Zimislecel)
One approach dives into the realm of stem cell–based therapy, specifically using zimislecel, a stem cell–derived islet cell infusion. This phase 1‑2 trial infused participants with either a partial or full dose of zimislecel, aiming to evaluate safety and restoration of physiologic insulin function. Findings were promising: all 14 adult participants who underwent the procedure showed evidence of engraftment and functioning islets (via detectable C‑peptide), signaling a potential breakthrough in beta‑cell restoration (PubMed).
2. Gene-Edited Allogeneic Transplants
Another pioneering strategy involves genetically modifying donor islet cells to evade immune detection, likely through downregulation of rejection markers and boosting CD47 “don't‑eat‑me” signals. In a notable case report, such edited islets were transplanted into a patient’s forearm muscle, where they engrafted and produced insulin without triggering an immune response—even without ongoing immunosuppression (Live Science).
Why This Matters
- Independence from injections and immunosuppression: Both methods aim to restore natural insulin production, potentially reducing or eliminating the need for lifelong injections and harmful immune‑suppressing drugs.
- Two complementary avenues: Stem cell methods promise scalability and patient-derived materials; gene editing offers targeted immune evasion for transplants.
- Early yet hopeful: While both studies are preliminary, they lay strong groundwork for future, larger trials.
Challenges Ahead
- Long‑term durability remains unknown—how long will the transplanted or infused cells survive and function?
- Safety concerns, including immune responses or rare adverse events, must be rigorously monitored.
- Scalability issues: stem cell production and biotech manufacturing must address costs, accessibility, and regulation.
- Regulatory and ethical hurdles—especially with gene‑edited cells—will shape the path forward.